It might be poor blood circulation if you’ve ever dealt with swelling, skin color changes, or even throbbing pain in your extremities. Often experienced in the arms, hands, legs, and feet, this condition could indicate more serious health issues.
Poor circulation can lead to complications such as varicose veins, blood clots, wounds, or even amputation. While consulting a healthcare provider is crucial, there are also steps you can take to improve circulation.
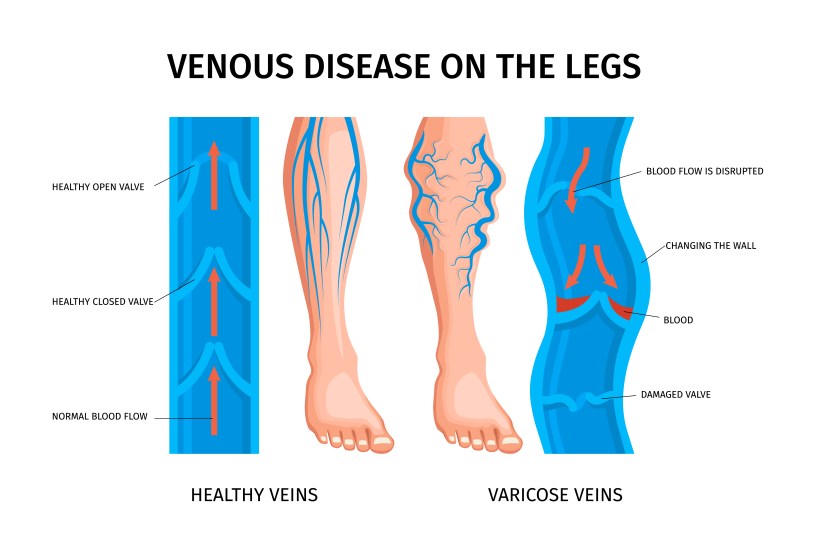
Conditions like peripheral artery disease (PAD) and chronic venous insufficiency (CVI) affect circulation significantly. In CVI, for instance, the veins’ valves in the legs don’t function efficiently, causing blood to pool and leading to various symptoms.
Some of the more distressing symptoms linked to poor circulation include:
- Muscle pain or weakness; a heavy feeling in the legs.
- Prickling sensations or a feeling of “pins and needles.”
- Skin appearing pale, blue, or abnormally red and inflamed.
- General leg swelling or painful swollen veins.
- Numbness.
However, there are proactive measures you can take to improve circulation, even if you’re dealing with peripheral artery disease (PAD) or chronic venous insufficiency (CVI).
Tips to Improve Circulation:
- Exercise: Physical activity benefits those with poor circulation. Simple, low-impact exercises like walking or pool therapy can significantly enhance vascular health. During exercise, your arteries release nitric oxide, which relaxes blood vessels and improves blood flow. Supervised exercise therapy may also help reduce leg pain.
- Dietary Changes: Adjusting your diet is critical for improving circulation, especially when combined with exercise. Reducing salt intake is paramount as high salt levels can cause fluid retention, increasing blood pressure and swelling. Embracing a Mediterranean diet can also be beneficial, offering heart-healthy perks such as a reduced risk of heart attack or stroke.
- Leg Elevation: Elevating your legs can aid circulation, especially for CVI patients. It would help if you are still exercising, but also find time to elevate your legs when resting. This allows the blood to move more effectively, using gravity to your advantage.
- Smoking Cessation: Quitting smoking is crucial as nicotine tightens blood vessels, restricting flow and leading to inflammation and arterial damage.
- Use of Compression or Diabetic Socks: Consult your healthcare provider to determine if diabetic or compression socks could benefit your health needs. Diabetic socks minimize skin irritation and prevent injuries, making them ideal for individuals with neuropathy who are at a higher risk of foot injuries due to reduced sensation. These socks are typically non-constricting with minimal seams and are made from materials that keep feet dry, reducing the risk of infection. On the other hand, compression socks provide graduated pressure on the legs to aid in blood circulation. The elastic in these socks helps reduce swelling. It prevents the accumulation of blood in the veins, known as venous pooling, which can lead to varicose veins and other circulatory problems. By improving blood flow, compression socks not only help to alleviate discomfort but also enhance overall leg health, reduce fatigue, and even improve performance in activities requiring prolonged standing or sitting. Whether for daily wear or specific medical conditions, both socks offer significant health benefits and can be crucial in managing symptoms of poor circulation.
- Medication: Consult your healthcare provider about medications that can aid your circulation, including statins, antiplatelet drugs, or blood thinners. In some cases, they might also recommend surgery to address blocked arteries or remove blood clots.
While natural remedies can significantly help, seeking professional advice for persistent or severe symptoms is important. Consulting your healthcare provider ensures you receive tailored treatment to manage your symptoms effectively.